Featured In





About Us
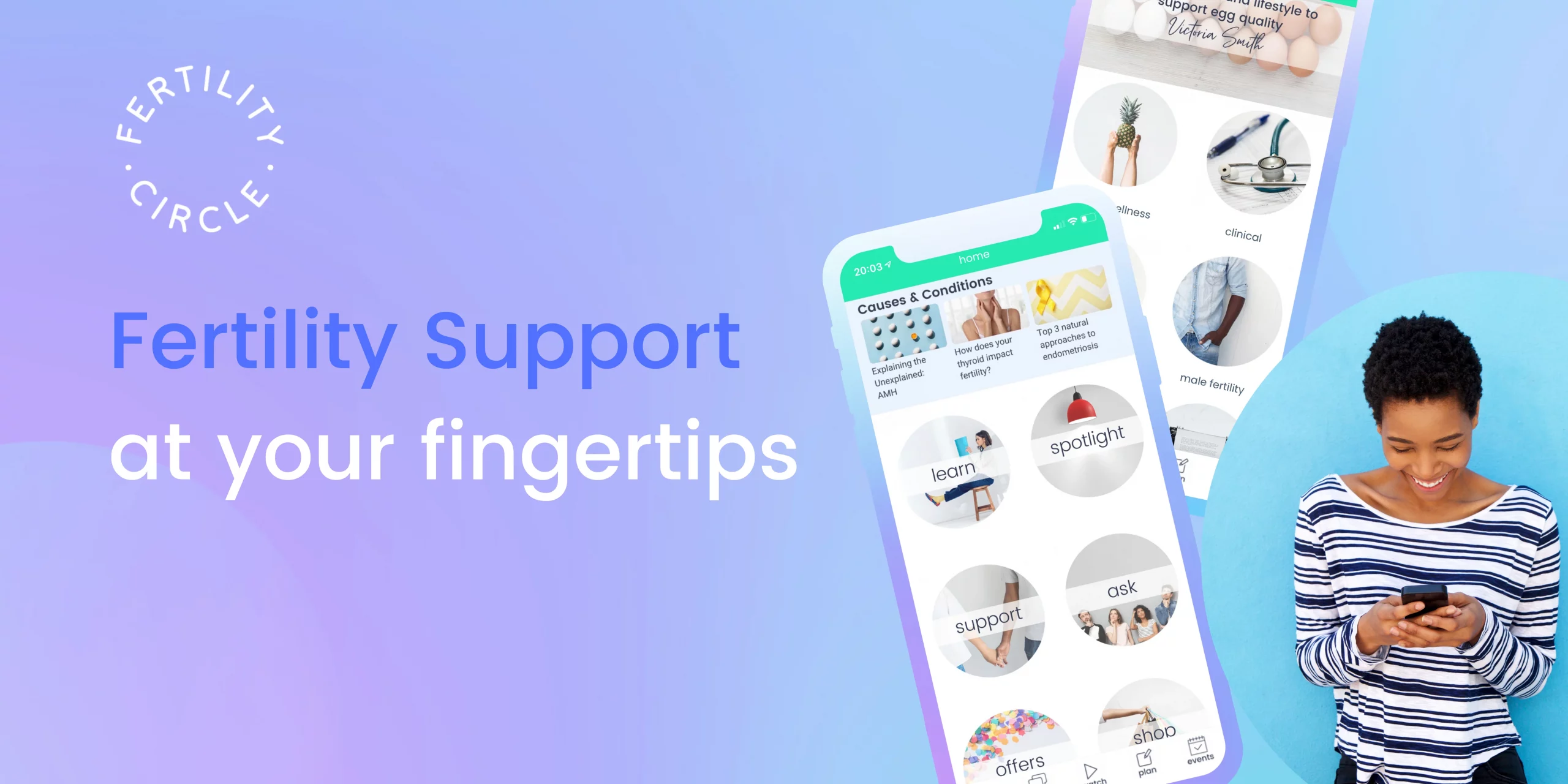
Hey! Welcome, we’re so pleased you’re here. We’re Abi, Karen and Jo, the co-founders of Fertility Circle. We’ve been on the fertility rollercoaster (and in fact as we write this we’re right back on it) - we’ve felt the rush of hope and the familiar stomach lurch of another miscarriage or failed cycle. Our paths crossed at just the right moment to spark an idea for a new kind of fertility platform – one that offered all the things we longed for when we were trying. That left us feeling empowered, not powerless. It seemed the available sites and sources were either heavily medical, leaving us even more bamboozled, or forums offering gems of the ‘my-sister-told-me-if-you-do-it-in-the-garden-when-the-moon-is-waning-you’ll-definitely-get-pregnant’ variety. Why wasn’t there a single place – a one-stop fertility shop, if you like – that was both practical (want to search for and book a clinic or holistic practitioner near you? No problem!) and supportive (would you like to connect with our community and read real life stories people who’re facing similar challenges to you? Come on in!). Fast forward a year and here it is – the Fertility Circle app - bringing the world of fertility to your fingertips. We hope it will become the definitive home of all things fertility. Our vision for this is to give you all you need to feel connected, empowered and supported, throughout your fertility journey. Our hope is that it will be a place for virtual hugs and support where you can come when you need a friend who just “gets it”. P.S. It's important to remember that this app and all content provided by Fertility Circle and its partners is for informational purposes only. It is not a substitute for medical advice, diagnosis or treatment.
Experts
Get support from best-in-class experts via top notch content, ask the expert and expert-led events
For Partners
List your business in our Directory
This is the go-to guide for finding fertility support. Users will be able to search for clinics and practitioners local to them or anywhere in the world. Don’t miss out and get your business listed.
List your fertility event in our Events feed
We try to source as many events as we can but we’re not aware of everything so please do get in touch so we can list your event. If you’re planning more of a casual meet up, you can list this yourself in the Community>Meet Ups section.
List your offer in our Offers section
Have a promotion, competition or special offer you’d like to promote? We’ll provide a coupon in our Offers section and help you get it out there through in-app promotion.
List your product in our Shop
We only list the very best fertility products so our users have a limited selection of the cream of the crop. We operate an affiliate model and also offer discounts to our premium Club members.
Contribute content to our Learn section
This is our content library covering a wide range of fertility topics. Writing articles or creating video is a great way to increase exposure for your business and share your knowledge and the topics you care about.
Apply to become one of our Resident Experts
These are our go-to experts who support our community. You’ll see their names popping up around the app. Being an expert means you’ll become a trusted voice, which is great for your business. You can find out more by heading to become one of our experts in the side menu of our app.
And the best part, all of this is FREE as we’re in our launch phase. Activate now to take advantage of this amazing offer.
How to activate?
Just fill in the partnerships survey here telling us how you'd like to get involved and we'll be in touch with more info asap!
Community
Join a growing like-minded community of people that get you
Free Fertility Wellness Pack
Sign up to our newsletter and get our FREE Fertility Wellness Pack full of tips to support your fertility journey as well as special offers, competitions and exclusive content
Discover
Find all the best fertility info, events, products and much more

What are people saying




Introducing The Fertility Circle
Magazine
-
Ask the Experts: Naava Carman shares her top tips as fertility treatment resumes
Here Naava Carman, from The Fertility Support Company, answers questions from our audience and shares her top baby-making tips. https://www.youtube.com/watch?v=SRKStDAhRlA
-
Ask the Experts: Victoria Smith Nutrition on nutrition for fertility
Here one of our Expert Panel members, Victoria Smith Nutrition, answers questions from our audience on all things fertility nutrition from the impact of caffeine,
-
Fertility 101: IUI – how it works
What is IUI? During IUI, the best and strongest-looking sperm are selected, by doctors, from a sample of your partner’s sperm (or your donor’s sperm if
-
Fertility stories: Katy
Katy's story Hey, I’m Katy - a Healthcare Assistant living in Devon. I’m sharing my story in the hope that it can help others and raise